Health and Wellness
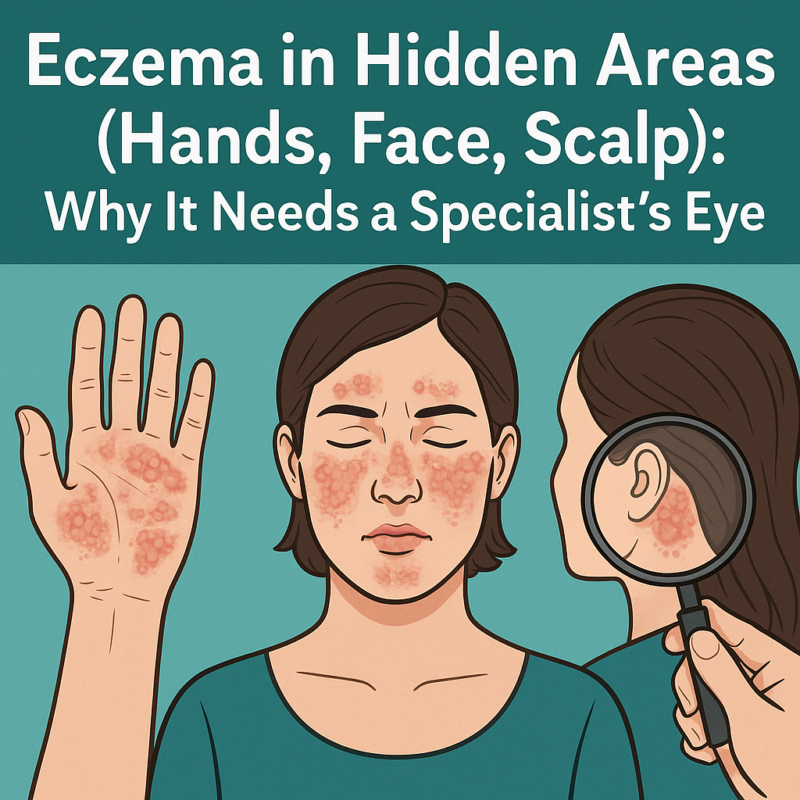
Eczema in Hidden Areas (Hands, Face, Scalp): Why It Needs a Specialist’s Eye
Introduction
Can your eczema location reveal what’s triggering it? Hand eczema disrupts the skin’s barrier function through repeated exposure to irritants and water, while facial eczema responds differently to standard topical steroids due to thinner skin absorption rates. Scalp eczema mimics other conditions like seborrheic dermatitis and psoriasis, requiring diagnostic techniques for accurate identification. These anatomical variations require different treatment approaches — what works on body eczema may affect symptoms differently in these sensitive areas.
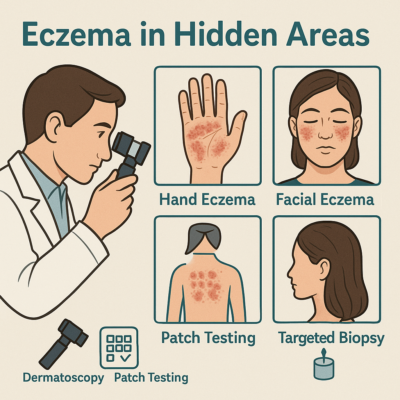
If your symptoms are persistent or difficult to control, seeking help from a dermatologist Singapore for eczema ensures you receive an accurate diagnosis and treatment tailored to your skin type and affected area. A specialist can use diagnostic tools including dermoscopy, patch testing, and targeted biopsies to differentiate between eczema subtypes and rule out other conditions that mimic eczema in these regions.
Hand Eczema
Hand eczema develops through multiple pathways — irritant contact dermatitis from repeated water exposure, allergic contact dermatitis from specific substances, or atopic hand eczema linked to underlying atopic conditions. The hands’ constant use and exposure to environmental factors creates a cycle where damaged skin barriers allow increased irritant penetration, triggering inflammation that further compromises barrier function.
Occupational factors significantly influence hand eczema patterns. Healthcare workers develop eczema from frequent handwashing and glove use, with latex proteins and rubber accelerators acting as both irritants and allergens. Hairdressers face exposure to para-phenylenediamine in hair dyes and glyceryl thioglycolate in permanent wave solutions. Food handlers encounter proteins that penetrate wet, macerated skin, while construction workers react to chromates in cement and epoxy resins.
Patch testing identifies specific allergens in hand eczema cases, with standard series testing revealing reactions to nickel (door handles, tools), fragrance mix (soaps, lotions), and methylisothiazolinone (preservatives in wet wipes and cleansers). Extended series testing targets occupation-specific allergens — rubber additives for healthcare workers, hairdressing chemicals for stylists, and food allergens for kitchen staff.
Treatment requires both protective and therapeutic measures. Barrier repair involves ceramide-containing moisturizers applied immediately after water exposure, with ointments providing occlusion compared to creams. Topical calcineurin inhibitors offer steroid-sparing options for maintenance therapy, particularly useful for finger web spaces and palmar surfaces where steroid-induced atrophy poses risks. Phototherapy using targeted UVB or PUVA delivers controlled doses to thickened palmar skin that resists topical penetration.
Facial Eczema
Facial eczema requires different management due to the face’s unique skin characteristics — increased blood vessel density, higher sebaceous gland concentration, and thinner epidermal layers that enhance absorption of topical medications. Eczema treatments designed for body use can trigger perioral dermatitis, steroid-induced rosacea, or rebound flaring when applied to facial skin.
The differential diagnosis for facial rashes extends beyond eczema. Seborrheic dermatitis affects nasolabial folds and eyebrows with greasy scales, while rosacea presents with central facial erythema and pustules without scaling. Contact dermatitis from cosmetics creates patterns matching application areas — eyelid dermatitis from eye makeup, perioral dermatitis from lip products. Photodermatoses spare sun-protected areas under the chin and behind the ears.
Cosmetic ingredients frequently trigger facial eczema through both allergic and irritant mechanisms:
- Preservatives like methylisothiazolinone and formaldehyde releasers cause delayed-type hypersensitivity reactions appearing 24–72 hours after exposure
- Fragrances, including natural essential oils, provoke reactions in sensitized individuals
- Physical sunscreen ingredients like titanium dioxide rarely cause reactions, while chemical filters like oxybenzone act as photoallergens
Treatment protocols minimize steroid use through non-steroidal alternatives. Tacrolimus 0.03% ointment provides anti-inflammatory effects without atrophy risk, making it suitable for periocular and perioral areas. Pimecrolimus cream offers similar benefits with a lighter texture. When corticosteroids are necessary, low-potency options like hydrocortisone 1% or desonide 0.05% may be considered for short treatment courses. A healthcare professional should determine appropriate treatment protocols.
Scalp Eczema
Scalp eczema presents diagnostic challenges due to hair coverage obscuring visual examination and similar presentations among multiple scalp conditions. Seborrheic dermatitis produces yellowish, greasy scales along the hairline and crown, while psoriasis creates well-demarcated silvery plaques with bleeding points when scales are removed. Atopic dermatitis of the scalp causes diffuse dryness with fine scaling and intense pruritus.
Dermoscopy reveals distinguishing features invisible to the naked eye. Eczematous conditions show dotted vessels in regular distribution with yellowish scales and absent hair shaft abnormalities. Psoriasis displays regular dotted vessels with white scales and a uniform red background. Tinea capitis shows comma hairs, corkscrew hairs, and broken hair shafts with surrounding scaling.
Scalp eczema impacts hair growth through chronic inflammation, damaging follicular stem cells and causing temporary hair shedding. Severe scratching creates trauma resulting in broken hairs and traction alopecia. Secondary bacterial infections can progress to scarring alopecia if untreated. The inflammatory environment alters the hair cycle, pushing follicles prematurely into the telogen phase.
Vehicle selection determines treatment success:
- Solutions penetrate through hair but may increase dryness
- Foams spread easily with minimal residue
- Oils moisturize and soften scales but can feel greasy
- Medicated shampoos require adequate contact time before rinsing
💡 Did You Know?
The scalp contains numerous sebaceous glands that can become inflamed in eczematous conditions, creating a unique inflammatory environment compared to other skin areas.
Diagnostic Approaches
Dermatoscopy provides magnified visualization of skin structures invisible to standard examination. For hand eczema, dermatoscopy reveals vesicle formation and secondary infections. Facial examination identifies vascular patterns distinguishing eczema from rosacea or lupus. Scalp dermatoscopy differentiates scaling patterns, vascular arrangements, and hair shaft abnormalities across conditions.
Patch testing protocols vary based on triggers. Standard series includes allergens like nickel and preservatives. Cosmetic series targets facial eczema triggers including UV filters and fragrance components. Hairdressing series identifies reactions to hair dyes and styling products. Occupational series covers workplace exposures specific to each patient’s job.
Skin scrapings and cultures rule out infectious causes that mimic eczema, such as fungal infections or bacterial colonization.
⚠️ Important Note
Eczema herpeticum requires immediate antiviral treatment. Vesicular eruptions with punched-out erosions, fever, and lymphadenopathy indicate this complication — seek medical attention immediately.
Treatment Modifications by Location
- Hands: Occlusive therapy with cotton gloves enhances penetration. The “soak and smear” method maximizes hydration.
- Face: Use pH-balanced, fragrance-free formulations. Choose mineral-based sunscreens and green-tinted primers for redness.
- Scalp: Apply treatments directly to the scalp using a narrow-tip applicator. Leave-on formulations under shower caps can improve absorption.
✅ Quick Tip
Apply scalp treatments in sections, parting hair every 2 cm for even coverage without waste.
What Our Dermatologist Says
Location-specific eczema often signals underlying triggers patients may overlook. Hand eczema in one family member who does dishes while others remain unaffected suggests a contact allergen in dish soap rather than genetics. Facial eczema after new skincare routines points to ingredient sensitivity. Scalp eczema unresponsive to treatment may indicate yeast colonization requiring antifungal therapy.
Commonly Asked Questions
Why does my hand eczema worsen in winter?
Low humidity and indoor heating dry the skin. Switch to ointment-based moisturizers and wear cotton gloves overnight.
Can I wear makeup with facial eczema?
Yes — use fragrance-free, mineral-based cosmetics and remove them gently with micellar water.
Why does my scalp eczema cause hair thinning?
Inflammation disrupts follicles, pushing hair into shedding phase. Controlling inflammation restores regrowth over time.
How do I know if my eczema is infected?
Look for honey-colored crusting, tenderness, or fever. These signs require medical attention.
Should I get allergy testing?
Patch testing identifies contact allergens relevant to hand and facial eczema. It’s best done when eczema is under control.
Next Steps
Accurate diagnosis through dermatoscopy and patch testing identifies specific triggers affecting hands, face, and scalp. Location-based treatments improve outcomes and minimize side effects in these sensitive areas.
If you’re experiencing persistent hand eczema, facial redness and scaling, or scalp itching with hair loss, consult an MOH-accredited dermatologist Singapore for eczema for targeted evaluation and care.

For anyone in NYC dealing with these kinds of eczema flare ups, I do also recommend checking out Skin Center NYC – their clinical team works with science based, tailored dermatology treatments, which can be especially helpful for tricky or persistent eczema in sensitive areas https://skincenter.nyc/